
Osteoarthritis of the knee joint (deforming osteoarthritis of the knee joint, DOA, gonarthrosis) is called degenerative-dystrophic changes in the articular structures, in which the cartilaginous layer between the bone elements first thins and then collapses. In the early stages, the patient experiences discomfort and slight limitation of mobility, then the joint is deformed and, as the cartilage is destroyed, it completely loses its functions. Acute osteoarthritis is very painful and is accompanied by a significant decrease in the patient's physical activity. If the treatment of gonarthrosis of the knee joint is not started on time, the patient may become disabled.
For reference:According to statistics, one in five adults in the world suffers from osteoarthritis of the knee joint. Knee osteoarthritis can be unilateral or bilateral; In women, the pathology is diagnosed twice as often as in men. People over 45 years old often face the problem of joint deformation due to age-related changes in the body. If this diagnosis is made to young people, the cause is usually trauma.
Why does pathology develop?
The knee joint is one of the most complex in the human body. Bears most of the load when walking and other movements. It is not surprising that with age its elements begin to wear out and lose their functions. First, the cartilage layer in the articular joint loses its elasticity and elasticity, then it dries out and cracks. The shock-absorbing properties of cartilage are reduced, and this is precisely what causes discomfort and pain when moving: knocks and impacts of the articular structures against each other are no longer softened by anything, the bones are gradually exposed and rub against each other. .
Deforming osteoarthritis of the knee joint in old age is an optional phenomenon, it is not diagnosed in everyone. There are a number of provoking factors, the combination of which causes pathological changes in the joint.
The most common causes of pathology are the following:
- excess weight - the joint must withstand additional loads;
- Osteoporosis is a pathology in which the demineralization of bone tissue occurs;
- chronic diseases associated with metabolic disorders in the body;
- traumatic sports - gonarthrosis is often called the disease of football players due to frequent trauma to the knee joint;
- some types of professional activities associated with intense physical activity (osteoarthritis and osteoarthritis) are found in chargers;
- spinal injuries in which the distribution of loads on the joints of the lower extremities is disturbed;
- hereditary predisposition.

Articular cartilage does not wear away immediately. In the early stages, the manifestations of the disease are absent or insignificant, the patient does not consult a doctor and does not take any measures to stop the pathological process. But, if dystrophic changes are still identified, the patient has time to start treatment and prevent irreversible changes. To do this, it is first necessary to establish what the main signs of osteoarthritis of the knee joints are.
How to recognize the disease.
The symptoms of osteoarthritis of the knee joint become pronounced at the stage when the cartilage has already thinned and begun to deteriorate. Grade 1 gonarthrosis may not make itself felt for years. However, later, attentive patients remember that they still felt atypical symptoms, they simply did not attach much importance to them, since they were not constant and did not cause much discomfort.

You may suspect destruction and inflammation of the right or left knee joint based on the following specific signs:
- morning stiffness in the joint;
- limitation of mobility after a long stay in one position;
- discomfort in the knee when climbing stairs: burning sensation, hypersensitivity;
- night pain in the knees;
- pain after physical work or sports;
- Sudden periodic weakness of the lower extremities. If right-sided or left-sided gonarthrosis develops, only one affected leg gives way.
But still, the main symptom of the destruction of the knee joint remains pain. They can be of variable intensity and sometimes disappear. But as the pathologies progress, they appear more frequently, become more intense and bother the patient even at rest, in the absence of physical activity. Depending on the severity of the symptoms, the doctor can diagnose what stage the disease is in.
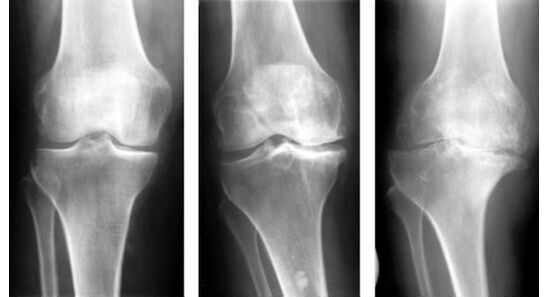
- Manifestations of pathology in stage 1:pain is not yet a concern, the patient may notice rapid fatigue when engaging in sports or physical activity, a slight limitation of joint mobility after prolonged rest. An x-ray will show a slight narrowing of the space between the bones of the joint, an uneven surface of the cartilage with slight compactions.
- For gonarthrosis of 2 degrees.Symptoms appear brighter and more frequently. Usually the patient already understands that something is wrong with his knees. Joints hurt and "twist" when the weather changes, after physical exertion. Even the gentlest movements cause knee pain. If a person lets his legs rest, the pain will go away. But under load they will resume again. Also at this stage of pathology, there may be a characteristic crunch in the knee when bending and extending the leg, difficulty and pain when trying to bend the leg at the knee more than 90 degrees. An x-ray will show a change in the shape of the joint cup and the presence of fluid in the joint cavity.
- Gonarthrosis 3 degreesIt is characterized by severe pain that occurs regardless of whether the limb is loaded or at rest. The painful joint is especially painful at night and when weather conditions change. The patient can no longer bend his leg at the knee, so his physical activity and performance decrease. The x-ray clearly shows degenerative changes in the joint tissues. The deformation is also visible visually with the naked eye. The patient's legs are bent at the knees like the letter "o" or "x", which ultimately leads to the inability to move independently, without support, and even more so to perform usual professional and household tasks. The person becomes disabled.

Typically, patients consult a doctor in the second stage of the disease, mainly to find an effective medication for knee pain. In the first stage, it is quite difficult to identify gonarthrosis, since the symptoms are mild and only minor changes are seen on x-rays. Detecting pathological changes in the joint is possible only with a comprehensive examination.
Diagnostic methods
Diagnosis begins with a visual examination and questioning of the patient. What will indicate the possible development of gonarthrosis:
- enlargement and change in the shape of the knee joint;
- a distinctive crunching sound when the kneecap shifts;
- pain when palpating the joint;
- limitation of joint mobility.
In the early stages, degenerative changes in cartilage tissue may not be visible, so CT and MRI are additionally recommended. With the help of modern diagnostic techniques, the doctor can accurately determine the severity of the joint involvement, whether there is inflammation and fluid accumulation in the joint cavity, and also differentiate osteoarthritis of the knee joint from other pathologies.
Classification
In modern orthopedics, there are two main types of osteoarthritis of the knee joints:
- primary gonarthrosis;
- secondary gonarthrosis.
The primary form of the disease develops on its own due to age-related changes or metabolic disorders. Secondary is the consequence of another disease, injury or failed surgical intervention. Post-traumatic osteoarthritis of the knee joint can develop several months after a hematoma, subluxation, or fracture. Depending on the nature of the course, osteoarthritis is classified as acute or chronic. It is easier to cure the acute form of the disease.
Official medicine for gonarthrosis.
Complex treatment of osteoarthritis of the knee joint begins only after final confirmation of the diagnosis. If the patient's condition is not critical, doctors will first try to stop the progression of pathology with the help of medications. Physiotherapy, massage and manual therapy are used as additional methods.
The main objectives of complex therapy:
- relieve pain and discomfort;
- restore joint mobility;
- stop the destruction of the cartilage layer and, if possible, restore it.
The important points are physiotherapy and compliance with a special diet. There are exercises and products that work to restore damaged joint tissues and help restore mobility at least partially. If you consult a doctor in a timely manner, these measures are sufficient for the knee joint to begin to function fully again.
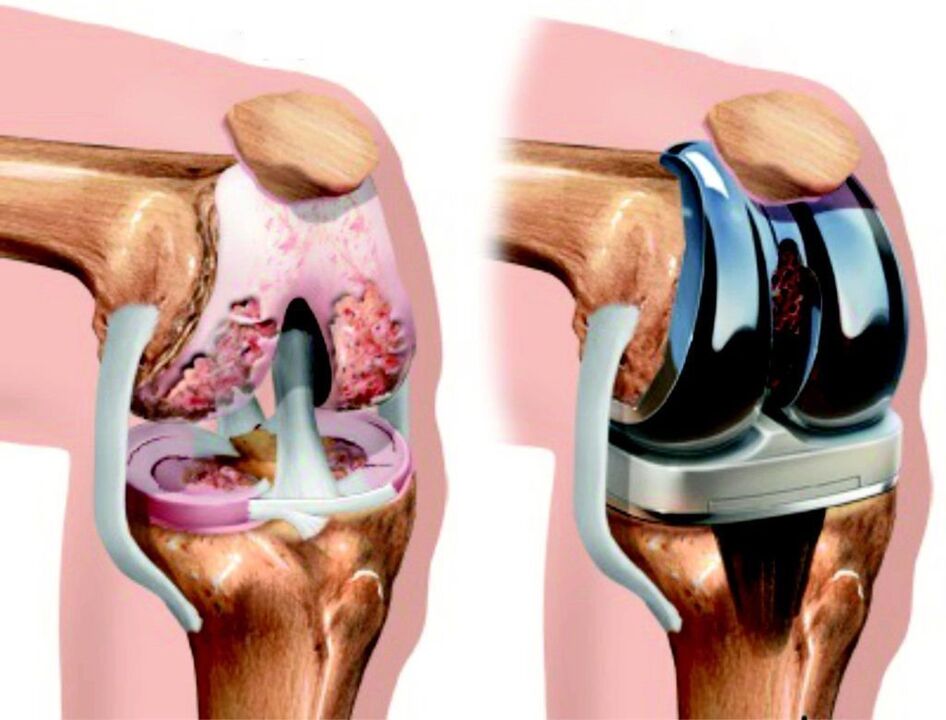
But if the disease has reached the third stage, the joint is severely damaged, even the most expensive drugs will not help to restore it. Surgery will be required to preserve at least partial function of the limb. It consists of removing the remains of the affected joint structures and implanting an implant, the procedure is called endoprosthesis.
Pharmacological treatment of gonarthrosis.
To eliminate unpleasant symptoms of the disease, restore and strengthen the joint, a complex of drugs of various groups and actions is used.
- Non-steroidal anti-inflammatory drugs– With them the treatment of the joints begins, they quickly relieve pain, swelling, fever and partially stop the inflammatory process. But they cannot be taken for a long time, since the active components of the composition have an extremely negative effect on the functions of the digestive tract and the composition of the blood. Typically, the course of treatment with NSAIDs lasts no more than 5-7 days. Medications can come in the form of tablets for internal use or in the form of ointments and gels for external use.
- Chondroprotectors– these are drugs that improve the nutrition of cartilage tissue and restore its firmness and elasticity. Chondroprotectors also partially relieve pain and swelling. But these medications don't work right away. The first effect will be noticed a few weeks after the start of treatment. It is recommended to take chondroprotectors for at least six months.
- Hormonal medications.They are also called corticosteroids. Medications containing hormones are used if the pain is very severe and the inflammation progresses even after treatment with NSAIDs. They are administered by injections intramuscularly or directly into the joint cavity. These drugs instantly relieve pain, reduce swelling and inflammation. But they have a number of contraindications and even more side effects than non-steroidal anti-inflammatory drugs, which is why they are prescribed in extreme cases. Hormonal drugs can be purchased in pharmacies only with a doctor's prescription. Immediately after the patient's condition improves, corticosteroids are discontinued.

The treatment is complemented with intra-articular injections of hyaluronic acid. This substance stimulates the production of synovial fluid, saturates the cells with moisture, restores their elasticity, firmness and prevents abrasion. The cost of the procedure is quite high, but the effectiveness is worth it.
On a note:Of all the drugs listed above, only chondroprotectors affect the cause of the disease. They stimulate the regeneration of destroyed cartilage tissue and prevent damage to surviving cartilage cells. But these drugs are expensive, and to obtain a noticeable and long-lasting effect, it is necessary to take them regularly for several months in a row, and sometimes even years. The cost of full treatment for many patients, especially retirees, is often prohibitive.
Unconventional treatment methods.
Patients who have experienced first-hand what knee osteoarthritis is and what unpleasant symptoms it manifests, always have several remedies available in case the pharmacy and medications are not available. People suffering from gonarthrosis and knee pain prepare tinctures, ointments and ointments based on medicinal plants in advance; almost all recipes require time and fresh raw materials, available only in the spring-summer season.
Treatment with dandelions.
There are several ways to strengthen the joint and restore its mobility, as well as get rid of unbearable pain with the help of this medicinal plant. The simplest is to eat five heads of dandelion every day during the flowering period. This should be done on an empty stomach, after rinsing the flowers with boiled water. A tincture for rubbing the joints is also prepared from dandelions.
The cooking recipe is as follows:
- Collect exactly 50 open dandelion heads.
- Place in a dark glass bottle with an airtight cap.
- Pour 300 ml of good vodka or triple cologne.
- Infuse away from sunlight for a month, shaking the container from time to time.
- Without expressing yourself, transfer it to the first aid kit, use it before going to bed to rub the sore knee, then wrap the joint with heat and lie down under a blanket.
There is another interesting recipe against osteoarthritis of the joints that uses dandelion. First you must collect the leaves of the plant and dry them. Then pour boiling water and let it steam for half an hour. The resulting mixture must be chewed slowly and carefully for the time necessary to take exactly 3 thousand steps.

Recipes with burdock
The simplest recipe:
- pick two or three tender leaves from the plant and rinse with cold water;
- Mash the leaves lightly to release the juice;
- Apply to the affected joint and secure with a bandage.
Store this "compress" overnight, remove it in the morning and discard the leaves. Repeat the procedure daily for three weeks.
To enhance the effect, traditional healers recommend lubricating the knee with cinquefoil oil before applying burdock. It's really easy to prepare. Two tablespoons of chopped cinquefoil are poured into 250 ml of any purified and fragrance-free vegetable oil. The oil should be preheated well, but not boiled. Leave the mixture for two weeks, then the oil can be used to treat joints.
Turpentine, eggs and other joint remedies.
With the yolk of a chicken egg you can prepare an effective massage for sore joints. It is prepared like this:
- Lightly beat one yolk in a bowl.
- Add a small spoonful of turpentine and stir.
- Then pour a large spoonful of vinegar and beat again.
The mixture is stored in the refrigerator and used before bedtime. After rubbing, the knee is wrapped in a warm cloth overnight. In the morning, you need to remove the bandage and rinse off the remaining product with warm water, and then apply any anti-arthrosis ointment.
Remember that all homemade preparations are effective only immediately after preparation, they are not stored for long (except for alcohol tinctures, they can be stored in a dark, cool place for up to six months). Don't expect instant results. Home remedies act on a cumulative system; Lasting relief will occur only after three to four weeks of regular use of home remedies for knee osteoarthritis. In the later stages, they will not be effective and will only help temporarily reduce pain and swelling.
Summary:Osteoarthritis of the knee joint, or gonarthrosis, is one of the most common injuries of the musculoskeletal system in older people. In young people it occurs after an injury or during excessive physical exertion. The disease can be completely cured only at stages 1-2 with a competent and comprehensive approach. In the third stage, most often it is necessary to resort to endoprostheses to at least partially restore the functions of the limb and prevent complications.

























